Hairline Lowering
typically 20’s - 30’s but any age Over 16; in women over 40, it creates a more youthful appearance; balances facial symmetry, reduces large forehead, corrects high hairline
Having a disproportionately high hairline or large forehead can divert attention from one’s otherwise balanced facial features and weigh heavily on a person’s self-esteem. Many of these individuals resort to wearing certain hairstyles that camouflage their high hairlines and would never consider wearing their hair styled backward in a ponytail. Genetics, hair loss or even prior surgery can all be causes for a high hairline. Unfortunately, many people who have a high hairline are unaware that a procedure exists for both women and men that reduces the size of the forehead and effectively lowers the hairline.
Also known as forehead reduction or hairline advancement, hairline lowering is both very effective and efficient at lowering the height of the hairline. The typical hairline begins somewhere between 5 to 6.5 centimeters above the brows, and a hairline above this height can cause the face to appear disproportionate.
As one of the world’s leading experts in the hairline lowering procedure, Dr. Champagne has performed the operation on patients from around the globe. He has co-authored a book chapter on the subject and truly enjoys seeing the instant gratification this procedure can bring to patients. There are many factors that play a role in surgical planning for hairline lowering including scalp laxity, hair thickness and density at the hairline, direction of natural exit of your hair and even previous surgery. This being said, the only absolute contraindication to forehead reduction is a previous coronal brow lift. The coronal brow lift is an older technique not used by Dr. Champagne in which an incision is made from ear to ear across the top of the head in order to raise the brow. During the procedure, a portion of scalp is removed and can actually raise the height of the hairline in the process. Because of this technique, blood flow to the hairline region can be at risk if hairline lowering surgery were to be performed, and therefore, patients with a prior coronal brow lift are not candidates for hairline advancement. Other factors such as density of hair at the hairline and natural exit of hair can be addressed and treated. For example, if you have thinning hair in the temple region, Dr. Champagne will usually recommend adding hair transplantation to improve density in that area. This can be performed either during the procedure or at a later date depending on your goals. In the event that you have minimal laxity to your scalp, you can still be a good candidate for hairline lowering. As a leading expert in forehead reduction, Dr. Champagne has successfully performed hairline lowering on many patients with tight scalp tissue without having to resort to using a tissue expander as many other surgeons would recommend. Every patient is unique, and therefore a detailed consultation with Dr. Champagne is necessary to discuss your goals and plan for your procedure. On rare occasion, patients who have minimal scalp laxity and very high hairlines may be candidates for a double procedure wherein a tissue expander is placed first followed by a second procedure 6-8 weeks later to remove the expander and lower the hairline. For those who live out of town and would like a consultation, Dr. Champagne is able to speak with you via videoconference to discuss your goals.
WHO IS A GOOD CANDIDATE FOR HAIRLINE LOWERING?
Good candidates for hairline lowering surgery include women with a naturally high hairline or large forehead who otherwise have thick hair and no personal or familial history of hair loss. Men with a high hairline or large forehead can also be good candidates for hairline lowering surgery if they have a thick hairline and no personal or family history of hair loss. Good scalp laxity is important, and therefore, a detailed consultation with Dr. Champagne is necessary.
WHAT TO EXPECT DURING YOUR INITIAL CONSULTATION:
Dr. Champagne will review your medical history and perform a physical exam. Be prepared to answer questions about current and past medical conditions. Talk about any medications you are currently taking or have taken recently, as well as any surgeries you have had. It is extremely important to tell us if you are allergic to any medications. To determine your treatment options and candidacy for hairline lowering, Dr. Champagne will examine and measure areas of your face including your forehead to determine overall symmetry and balance. In addition, you will take photographs for your medical record. During your consultation, Dr. Champagne will discuss with you your reasons for wanting forehead reduction and what your expectations are in terms of appearance after the procedure. You will also be able to view a large collection of approved before and after photos of Dr. Champagne’s patients.
PREPARING FOR A HAIRLINE LOWERING PROCEDURE:
Depending on your age and general health, certain preoperative tests may be necessary. We will discuss these with you and be sure that they are performed prior to undergoing surgery. If you are a smoker, Dr. Champagne will recommend that you stop smoking both before surgery and during your recovery period as smoking decreases blood flow in the skin and can slow the healing process. In addition, smoking increases the risk of tissue damage. By stopping smoking, you will improve your ability to heal and optimize your postoperative results. If you need help quitting smoking, we will be happy to assist you. Certain medications will need to be avoided both before and after surgery such as aspirin, anti-inflammatory drugs and herbal supplements, which can increase bleeding. We will provide you with a list of all medications to be avoided. For the day of surgery, you should also make plans for someone to bring you to and from the surgical center and stay with you at least the first night afterwards. If a caregiver is not available, or if you prefer to recover in privacy, our office staff will be happy to schedule postoperative care for you with our world-class postoperative care facility.
WHAT IS THE RECOVERY?
After a forehead reduction procedure, there can be minimal to moderate swelling in the forehead and scalp, and sometimes around the eye or cheek area. Most swelling diminishes over the first several days and is completely resolved within the first couple of weeks after surgery. Mild bruising can also occur around the eyes, but this is normal and does not interfere with vision. Numbness or reduced sensation should be expected around and just behind the hairline. This is temporary and is expected to resolve within the first few weeks to months. Many patients are healed enough to go back to work after a couple of days and can use a scarf or large hat for camouflage. Sutures placed at the hairline are removed by Dr. Champagne after one week.
OTHER BENEFICIAL PROCEDURES:
Those patients who undergo hairline lowering may also benefit from hair transplantation. In addition, a browlift can also be performed during the procedure if desired.
SCHEDULE A PERSONALIZED, CONFIDENTIAL CONSULTATION:
Please contact Dr. Jason Champagne to schedule a personalized, confidential consultation with our facial plastic surgeon, Dr. Jason Champagne. During your consultation, Dr. Champagne will address your goals and answer any questions you may have regarding hairline lowering or any other procedure we offer.
HAIRLINE LOWERING
Jason P. Champagne, M.D.
* The following is a chapter written by Dr. Jason Champagne and published in the highly recognized and respected textbook series Facial Plastic Surgery Clinics of North America.
SYNOPSIS: Hairline lowering or advancement, also known as forehead reduction, is a procedure that has been adapted and honed from scalp reduction and flap techniques. Although the high hairline can be found in both males and females of all races and ethnicities due to various diagnoses, hairline advancement is best suited for individuals, typically females, with a lifelong history of a high hairline and no familial or personal history of progressive hair loss. It is a procedure that is both effective and efficient in lowering the congenitally high hairline with very high patient satisfaction. Occasionally, a two-stage procedure will be required for the individual with a very high hairline or minimal scalp laxity. A thorough knowledge of the relevant anatomy and surgical limitations as well as a detailed history and physical exam is imperative to achieve desirable outcomes.
KEY POINTS:
The ideal patient for hairline advancement is a female with a congenitally high hairline and no personal or familial history of hair loss
A trichophytic incision is key to scar camouflage
Preservation of the occipital arteries is crucial
The average scalp can be advanced up to 2.5 cm especially if galeotomies are utilized
A two-stage procedure with scalp expansion prior to advancement is required in those with minimal laxity or significantly high hairlines
INTRODUCTION: Hairline lowering or advancement as a standalone procedure has its origins in maneuvers utilized for scalp reductions and flaps. Our experience is mostly for the purpose of correcting disproportion of the upper third of the face without browlifting in a younger patient group. The high hairline is more prevalent in certain ethnic and racial groups and is a source of self-consciousness that cannot be overcome with camouflaging hair styles. Patients perceive the problem as either a high hairline or a large forehead. The hairline lowering operation is both a very efficient and effective method of reducing the forehead with immediately noticeable results. The ideal patient for the hairline advancement procedure is typically female with a congenitally high hairline and no personal or familial history of progressive hair loss. A congenitally high hairline is one that causes the upper third of the face to be disproportionately greater than that of the middle and lower thirds. In order to achieve optimal results with a single procedure, potential candidates must meet specific preoperative criteria. Otherwise, a two-stage procedure is required with scalp expansion prior to hairline advancement in those with very high hairlines or minimal scalp laxity. This situation occurs in less than 10% of the author’s patients.
PREOPERATIVE ASSESSMENT AND PLANNING: To select appropriate patients for the procedure, the preoperative assessment should include a thorough examination of the scalp with a focus on evaluation of scalp laxity, direction of hair exit, and frontotemporal points and recessions. These key elements are not only important for choosing suitable candidates but also aid in preoperative counseling and patient decision-making. Forward-growing hairs at the hairline allow for hair growth through the scar and the highest probability of scar camouflage as will be discussed in greater detail later in the chapter. Patients with posteriorly exiting hairs at any point along the hairline, as seen in those with cowlicks, are informed that they might require future follicular unit restoration with either follicular unit transfer (FUT) or follicular unit extraction (FUE) to disguise the scar and achieve optimal results. Likewise, FUT or FUE is recommended for individuals who desire coverage of deep temporal recessions or advancement of acutely, downward-facing temporal hairs.
During preoperative consultation, a measurement of the height of the hairline should be taken. To help standardize the measurement, a point should be chosen at the glabella at the level of the interbrow region. From this point, the average female hairline should measure approximately 5 to 6.5 cm, and hairlines above this are generally considered high especially if they cause imbalance with the lower thirds of the face. Once the hairline has been deemed high, adequate scalp laxity can be determined by performing a simple maneuver with the fingers. A point is chosen over the forehead below the hairline and the fingertip is used to move the tissue as far superiorly as possible. The point of maximal tissue excursion superiorly is set to zero at the hairline from the glabella. The fingertip is then used to push the tissue downward from this point as far as possible, and a measurement is then taken between the two points. Also, the relative ease of moving the hair-bearing scalp forward and backward and the pinching of forehead skin aid in assessing how much the hairline can be lowered. This distance, which averages greater than 2 cm, very closely approximates the distance that the hairline can be advanced during a single-stage procedure and equates to a 25% reduction of the forehead in someone with an 8 cm hairline, for example.
Risks of the procedure as well as potential complications include bleeding, infection, telogen effluvium (“shock loss”) and scalp necrosis. In addition, specific problems relating to the post-operative scar include widening, visibility with future hair loss, hypo- or hyperpigmentation, and the possibility of needing a hair grafting session or scar revision to help camouflage the incision site. These scar problems rarely arise in the author’s experience. All patients are also informed that diminished sensation over the frontal scalp should be anticipated for 6 to 12 months in the postoperative period.
HAIRLINE MARKING: Preoperatively, the hairline should be marked just posterior to the fine vellus frontal hairs in a manner that creates an irregular, undulating pattern similar to those fashioned for routine hair transplantation. As the markings approach laterally to the downward-directed hairs of the temporal tufts, they should be curved posteriorly into the temporal hair for approximately 2 cm then inferiorly. It is important to create this marking in such a way as to avoid division of the posterior branch of the superficial temporal artery when performing the incision. The desired neo-hairline height is then chosen at a point over the forehead and a marking is made replicating the natural hairline above. A third marking can be drawn 0.5 to 1 cm above the anticipated neo-hairline to allow for a range of acceptable hairlines intraoperatively, and this should be discussed with the patient prior to surgery.
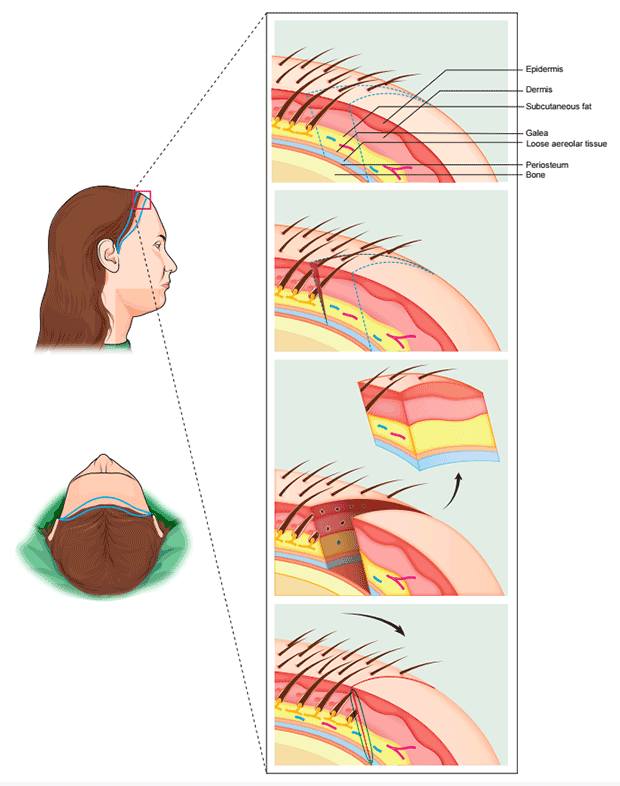
SURGICAL TECHNIQUE: After hairline marking, the patient is then brought into the operating suite and placed in the supine position with the head slightly elevated. In the author’s experience, the procedure is well tolerated with a combination of local anesthesia and intravenous sedation. The scalp and forehead are anesthetized in a ring-block fashion along with tumescence in a manner similar to that performed during an extensive FUT session. Once the scalp is well anesthetized, the incision is made at the hairline with a trichophytic approach, beveling at an angle that is approximately 90 degrees to the natural exit of surrounding hairs. This method is crucial for achieving hair growth through the eventual scar and providing optimal camouflage in the future (Figure 1).
FIGURE 1: Trichophytic hairline advancement. (upper left) Side view of hairline incision design. (lower left) Top view of hairline incision design. (right, top and bottom) (1) Hairline-scalp anatomy. (2) Superiorly the hairline incision is made by beveling forward at an angle approximately 90˚ to the natural exit of surrounding hairs. Inferiorly an incision is made over the forehead with the same beveled angle as that at the hairline. (3) Non-hair-bearing forehead tissue including skin, frontalis muscle and galea is fully excised. (4) The scalp is advanced forward to meet the forehead incision line. Transected follicles along the hairline incision line will eventually grow through the thin scar to provide camouflage along the length of the hairline.
Another important aspect of this incision is that it should include only the first 2 to 3 hairs behind the point where fine hairs of the anterior hairline transition into more coarse and dense follicular units. Slight modifications of the existing hairline shape can sometimes be made. The incision is carried to the subgaleal plane and transitions at the temporal hairline to parallel the exiting hairs as it is extended into the posttemporal hair. Bleeding is minimal due to tumescence, especially if care is taken to avoid the posterior branch of the superficial temporal arteries. Dissection can then be performed rapidly in the subgaleal, bloodless plane taking care to avoid injury to the occipital arteries posteriorly where visualization becomes more difficult. Undermining should take place posteriorly to the nuchal ridge, laterally to the limits of the galea, and anteriorly to a level approximately 3 cm above the brow in order to avoid lifting the brow in the process of wound closure. If the patient desires a brow lift, however, dissection can be easily carried inferiorly to release the brows, and superior advancement of the forehead flap is performed in the usual manner described for brow elevation.
Once fully elevated, the scalp is advanced, and the use of a D’Assumpção clamp or other flap-marking device helps determine the amount of forehead overlap. If the planned hairline height is not reached, galeotomies can be performed to allow for additional advancement. These are made with the use of a slightly bent, depth-controlled no. 15 blade to reach the more superficial subcutaneous plane while avoiding compromise to the blood supply of the flap. Electrocoagulation blades or needles should not be used for this. Each galeotomy provides a gain of 1 to 2 mm, and therefore, several parallel galeotomies may be required to achieve the desired hairline. After determining the level to which the scalp can be advanced, an incision is made over the forehead with the same beveled angle as that at the hairline while replicating the undulating pattern. Non-hair-bearing forehead tissue, including skin, frontalis muscle and galea, is then fully excised. One or two paramedian Endotines are then placed in the calvarium in a reverse direction to the usual placement during a brow lift at a 3- to 4-cm distance posterior to the neo-hairline. The scalp is then advanced with the use of 5-prong retractors over the course of 1 to 2 minutes to allow for tissue creep before securing the galea to the Endotines. The Endotines, in theory, help to relieve tension at the neo-hairline and work to allow the anterior 3 to 4 cm of scalp to be relatively compressed, thus distributing the subtle stretch of the scalp disproportionately and reducing the possibility of postoperative stretch-back. This anterior compression is thought to minimize splaying of follicular units and help maintain the full preoperative density at the hairline. The galea is then reapproximated using both 3-0 and 4-0 interrupted polyglycolic acid sutures, often with moderate tension, allowing for a tensionless fine closure at the skin edge. The skin is then closed with both 4-0 interrupted nylon sutures interspersed with surgical clips within the temporal scalp and 5-0 or 6-0 nylon or polypropylene sutures over the anterior hairline. Meticulous attention is given to the beveled skin closure at the hairline utilizing loupe magnification to ensure appropriate overlap of the de-epithelialized hair follicles. An evacuation drain has not been found to be necessary due to the amount of tension on the scalp and the resultant lack of subgaleal dead space. On infrequent occasions follicular unit grafts can be performed in the same sitting with donor material harvested adjacent to the intratemporal closure line. These grafts are only used in front of the temple hairs to narrow a wide forehead.
POSTOPERATIVE CARE: Immediately postoperatively, long-acting local anesthesia is injected along the incision line to provide patient comfort, and a pressure dressing is placed. On the following day, the dressing is removed, and patients can resume most non-strenuous activities within the first 24 to 72 hours. Edema is minimal, and periocular and forehead ecchymosis is rare, which is attributed to the strong, layered closure. However, a concurrent brow lift does increase the likelihood of periocular edema and bruising. Because tension is borne by the deep closure, removal of skin sutures and clips is permitted within 5 to 7 days. Due to the initial incision, there is minimal prolonged discomfort from the operation as the scalp is insensate for 6 to 9 months postoperatively, also allowing for the Endotines to be very tolerable. They should be long dissolved by the time sensation returns; hypoesthesia has resolved in all cases to date.
TISSUE EXPANSION: Preoperatively, if the scalp is noted to have minimal laxity or the amount of advancement required to achieve a desirable hairline height is beyond the average 2 to 2.5 cm, a 2-stage procedure is recommended. The 2-stage procedure involves the initial insertion of a tissue expander with expansion of the scalp performed gradually over the following 4 to10 weeks using similar methods as those described in the literature. During the expansion period, patients have concealed their ever-enlarging scalps with adornments ranging from wigs to oversized hats. A second procedure, which, with the exception of removal of the expander, is exactly as that described earlier, takes place when desired expansion is achieved.
SUMMARY: With attention to detail and careful preoperative planning, the single-stage hairline lowering procedure performed on a scalp with average laxity will allow for up to 2.5 cm of advancement with excellent long term results. Very lax scalps have allowed for up to 3.5 cm advancement with this one-stage approach. This brief (1.5 hour) operation, which in the author’s experience has no more morbidity than an extensive FUT/FUE session, moves an average of 3000 follicular units at one time. The 2-stage procedure, despite having the disadvantages of prolonged, progressive deformity and the cost of an additional operation, is still efficient and cost-effective considering the fact that up to 12,000 follicular units can be advanced. Either procedure is generally well-tolerated with minimal morbidity, and the end result, whether achieved through a one-staged or 2-staged approach, has been met with excellent overall patient satisfaction.